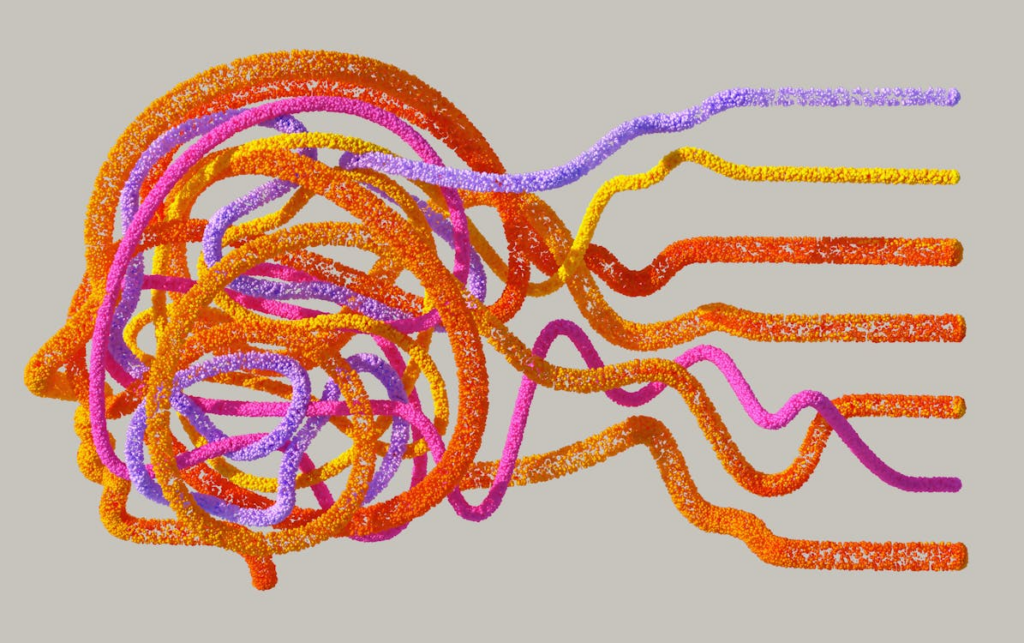
Many experts in psychiatry acknowledge that neuroscience advances have not yet transformed clinical practice. Yet, the public often hears that mental disorders stem from brain diseases cured by medication. So, how does this misleading narrative take shape? Research reveals that biases in scientific publishing, media oversimplification, and funding pressures distort the way we discuss mental health—with real consequences for patients.
How Biomedical Neuroscience Research Gets Misrepresented
Academic studies frequently highlight exciting early findings while downplaying contradictory or inconclusive results. Journals favor groundbreaking initial studies, even if later research disproves them. Media outlets then amplify these findings, rarely circling back when new evidence emerges.
Several key factors fuel this cycle:
- Publication Bias – Researchers and journals prioritize positive results over null or negative findings.
- Overstated Conclusions – Early-stage studies often make bold claims before thorough replication.
- Media Hype – Journalists, eager for breakthroughs, present tentative findings as definitive truths.
This creates a persistent myth: that mental health struggles boil down to simple biological causes, solvable only with medication.
Why the Neuroscience “Brain Disease” Narrative Harms Recovery
Viewing mental illness purely through a biological lens can backfire. Studies show that when people believe disorders like depression or anxiety stem only from brain chemistry, they:
- Grow more pessimistic about recovery.
- See patients as fundamentally different, increasing stigma.
- Overlook psychotherapy and social support, even though these approaches often work as well as—or better than—medication alone.
While psychiatric medications help many people, they don’t work for everyone. True healing requires a biopsychosocial approach, integrating biology, psychology, and social factors.
Therapy and Social Support: Powerful (But Underrated) Tools
Treatments like Cognitive Behavioral Therapy (CBT), EMDR (for trauma), and mindfulness-based therapies have strong scientific backing. Telehealth has made these options more accessible than ever, allowing people to get help from home. Yet, public discourse still leans heavily toward medication-first solutions.
Social factors—like strong relationships, financial stability, and community connections—also play a huge role in mental well-being. Ignoring them in favor of a purely biomedical model limits recovery.
A Better Way Forward: Balanced Mental Health Conversations
To improve care and reduce stigma, we need a more honest, nuanced discussion about mental health—one that:
- Acknowledges the limits of neuroscience in explaining mental illness.
- Values therapy and social interventions alongside (or sometimes instead of) medication.
- Emphasizes scientific uncertainty, since early findings often change.
By moving beyond reductionist thinking, we can offer patients truly effective, personalized care—not just a one-size-fits-all solution.
Looking for the best EMDR, CBT, and DBT therapist? Dr. Sara C offers highly rated telehealth services in Newport Beach, CA; Beverly Hills, CA; San Diego, CA; Portland, OR; Jacksonville, OR; Dallas, TX; and Houston, TX. Experience top-quality therapy from the comfort of your home.
In case of a mental health emergency, please call 911 or seek immediate professional help.
Source:
Dumas-Mallet, E., & Gonon, F. (2020). Messaging in Biological Psychiatry: Misrepresentations, their causes, and potential consequences. Harvard Review of Psychiatry, 28(6), 395–403. https://doi.org/10.1097/hrp.0000000000000276
